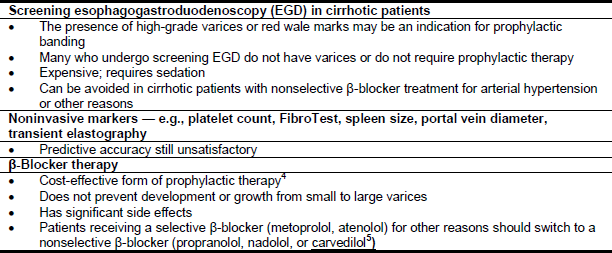
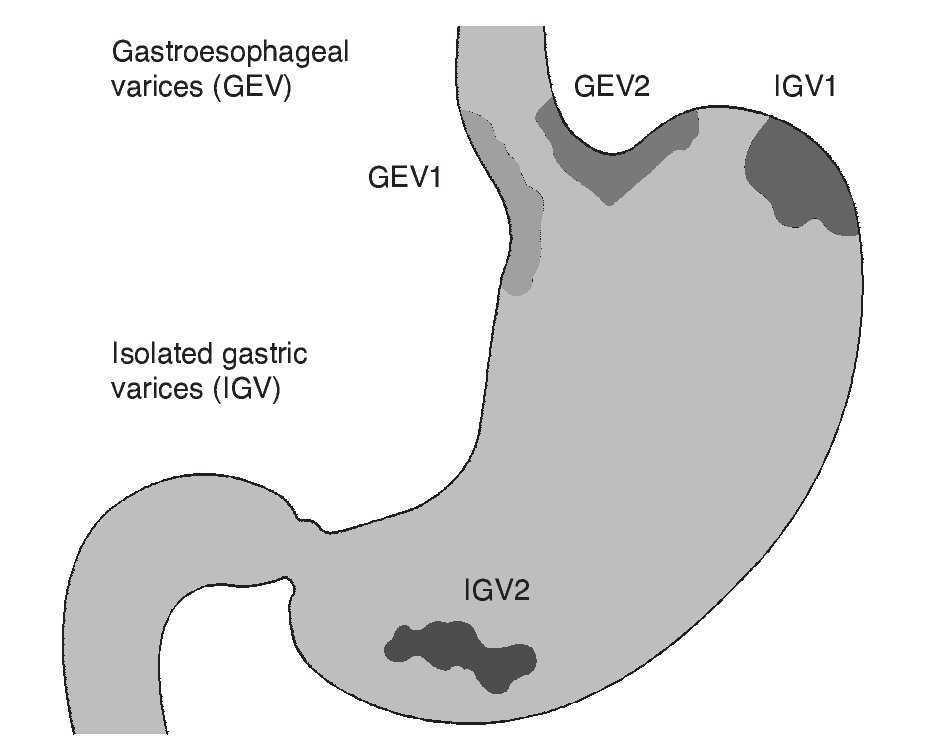
Take Quiz Thyroid disease and primary biliary cholangitis complications Take Quiz Endoscopy timing in patients with peptic ulcer bleeding Take Quiz Pancreatic cancer & gene mutations Take Quiz Screening of proximal advanced SARIN CLASSIFICATION FOR GASTRIC VARICES The Sarin classification of gastric varices identifies two types of gastro esophageal varices where esophageal varices are found concurrently two types of isolated gastric varices, found in the absence of esophageal varice (AASLD) includes a recommendation to simplify this using 2 grades (small andGastroesophageal varices (GEV) often refer to esophageal varices with gastric component Sahney A Oesophageal and gastric varices historical aspects, classification and grading everything in one place American Association for the Study of Liver Diseases/American College of Gastroenterology (AASLD/ACG) grading

Practice Guidelines sld
Aasld classification of esophageal varices
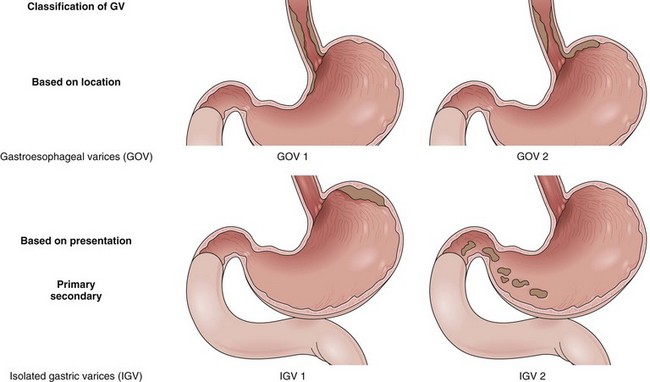
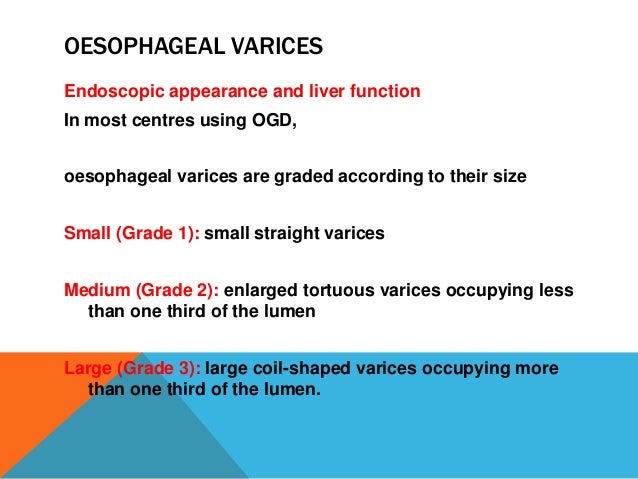
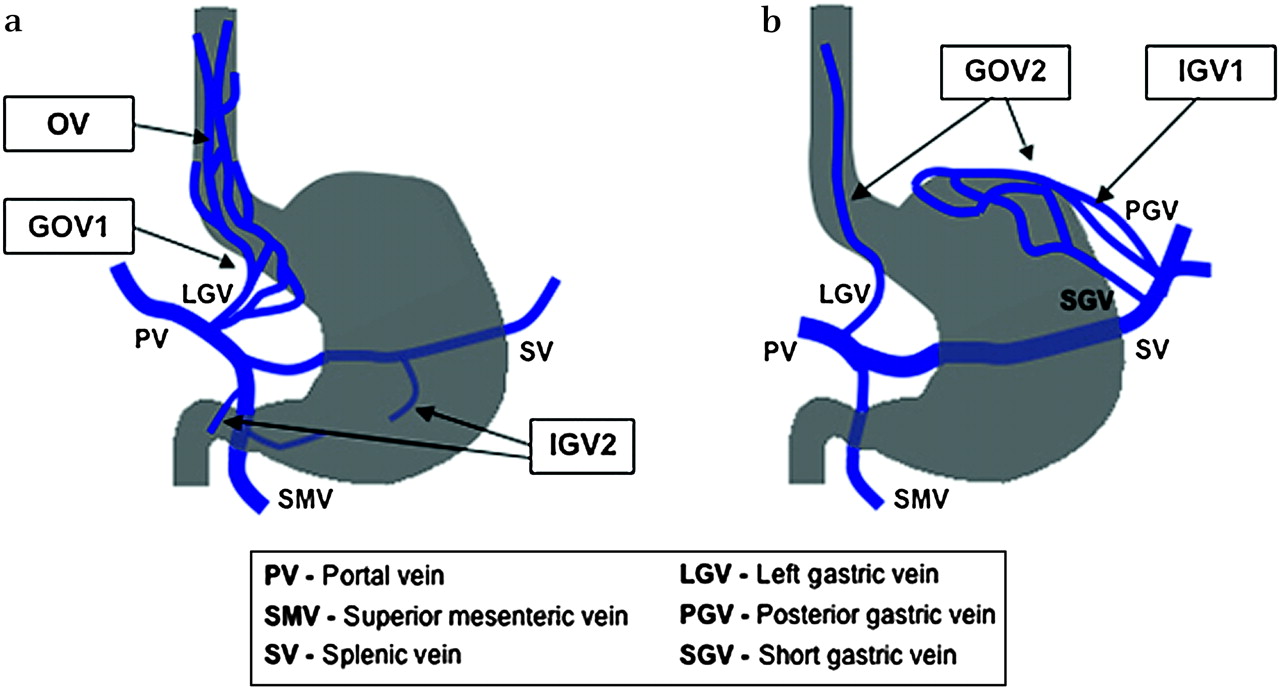
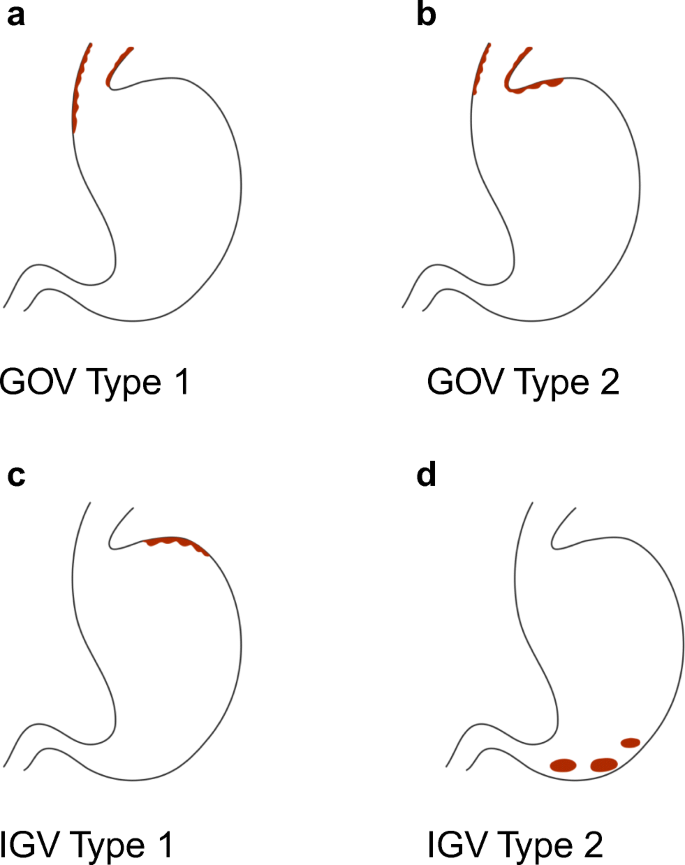
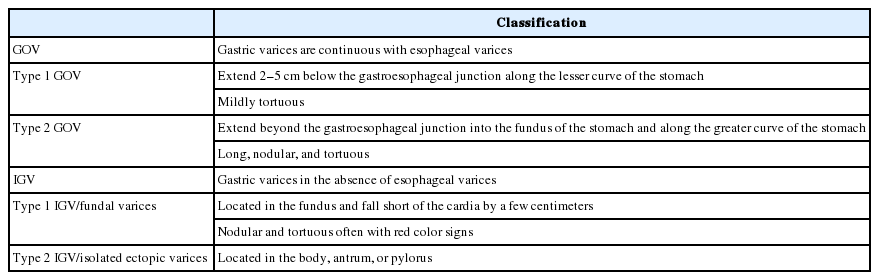
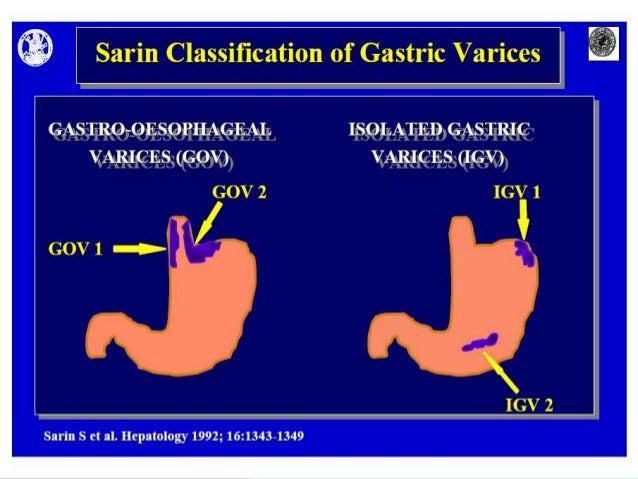
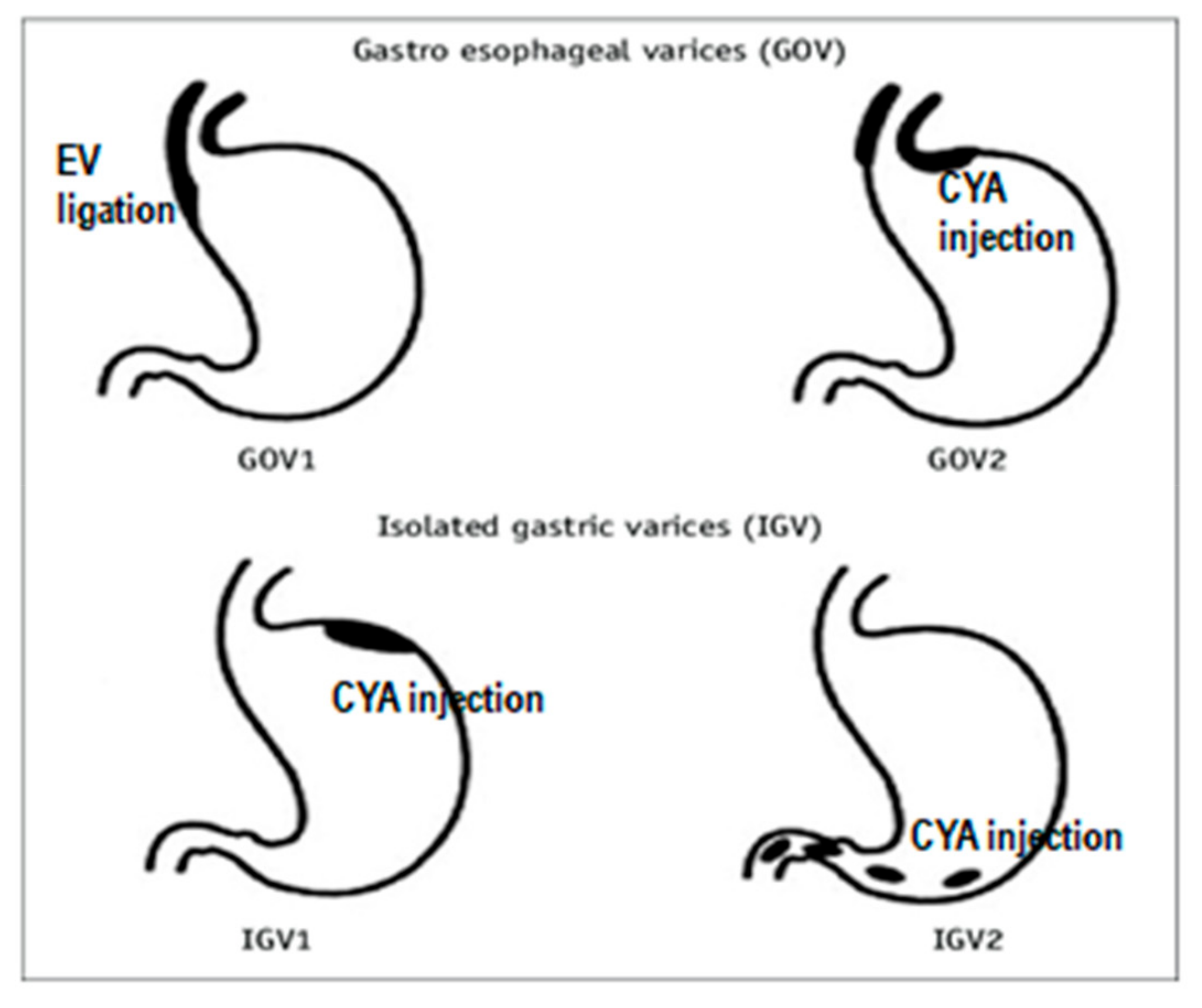
Aasld classification of esophageal varices- varices present in about 50% patients with cirrhosis correlated with severity of liver disease (more common in patients with ChildPugh class C) 1; Oesophageal and gastric varices classifications 1 SARIN CLASSIFICATION FOR GASTRIC VARICES The Sarin classification of gastric varices identifies two types of gastro esophageal varices where esophageal varices are found concurrently two types of isolated gastric varices, found in the absence of esophageal varice 2



Www Idsociety Org Globalassets Idsa Topics Of Interest Emerging Clinical Issues sldguidelinehccupdate10 1 Pdf
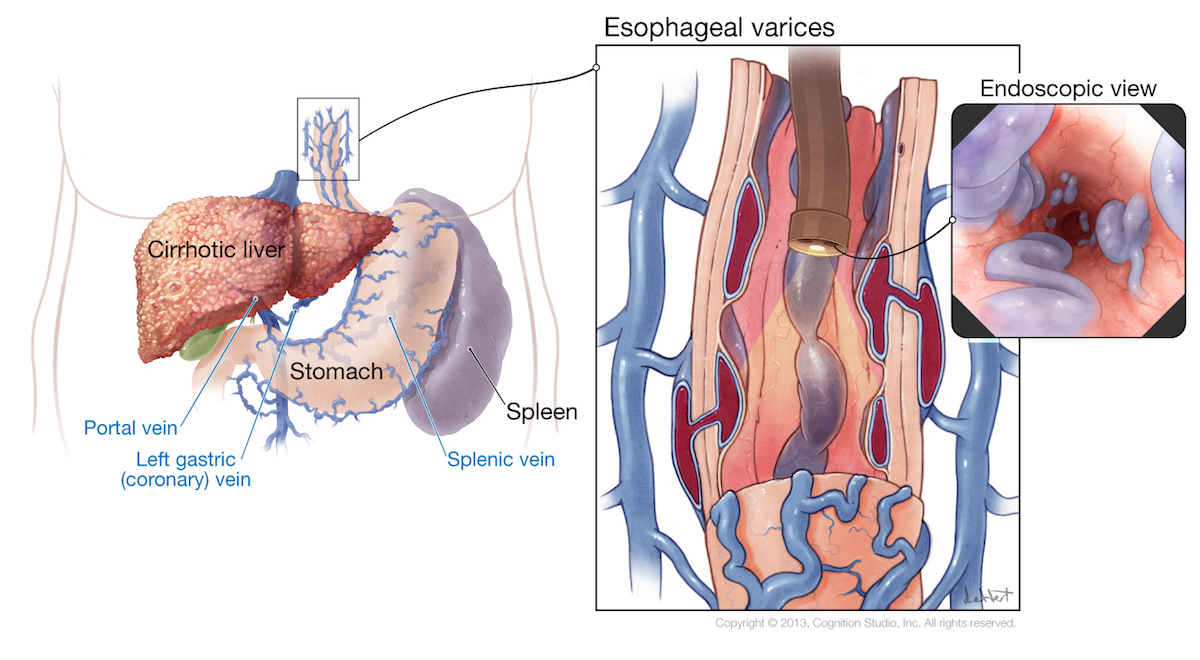
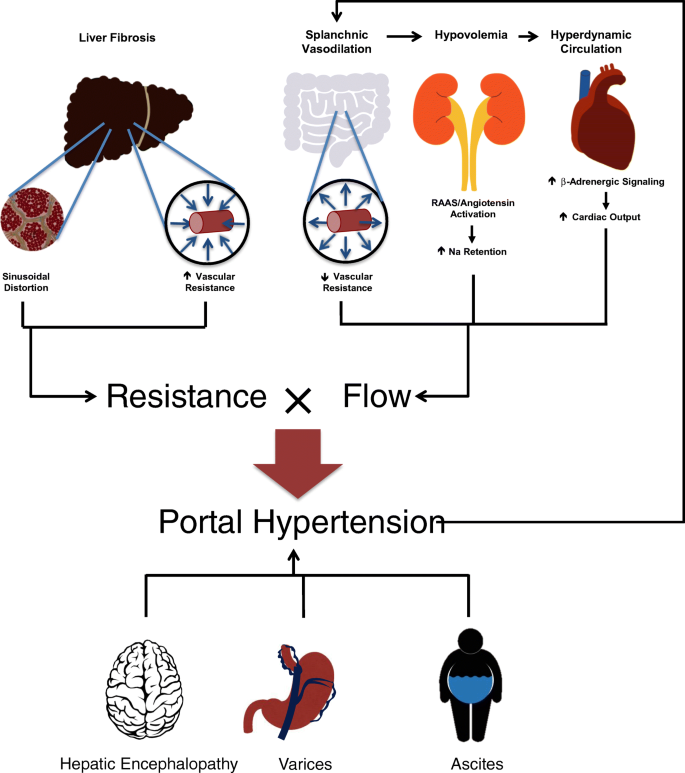
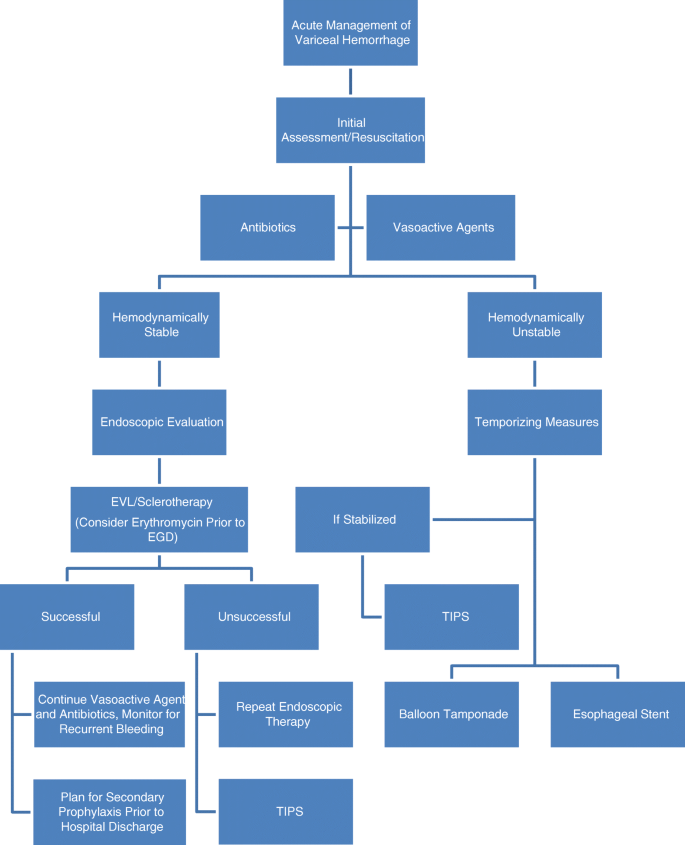
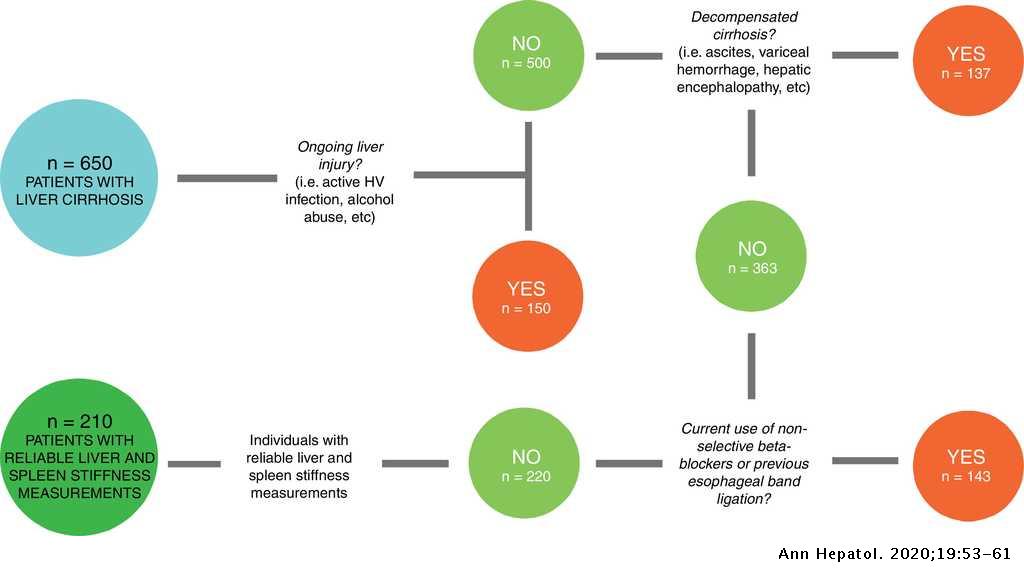
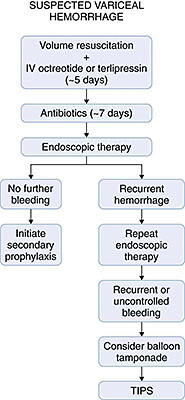
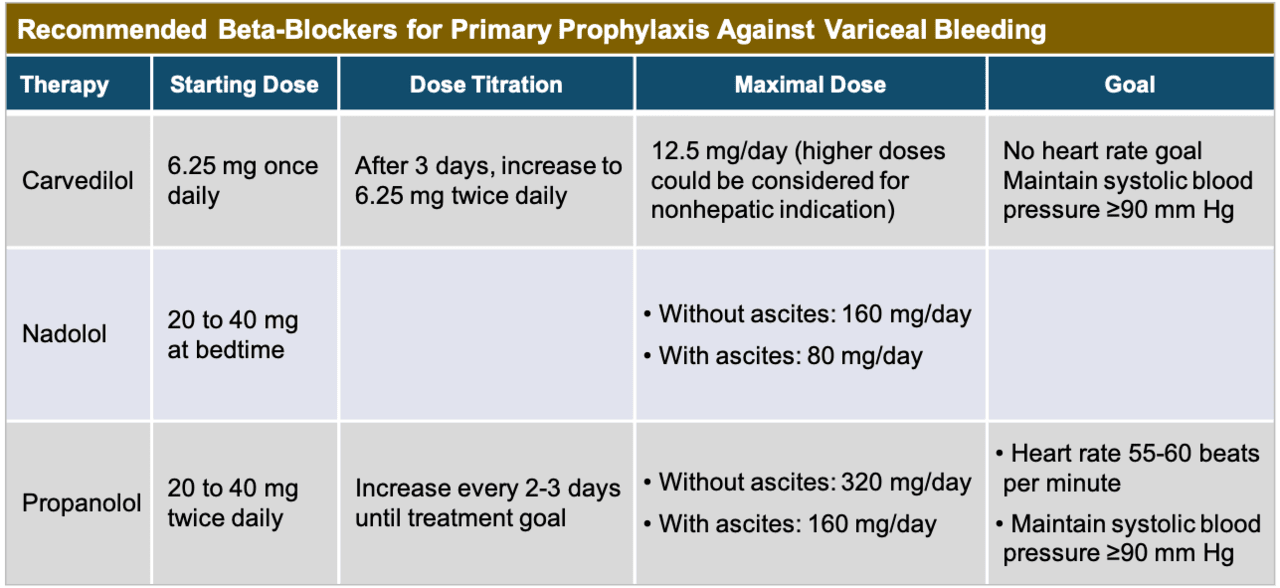
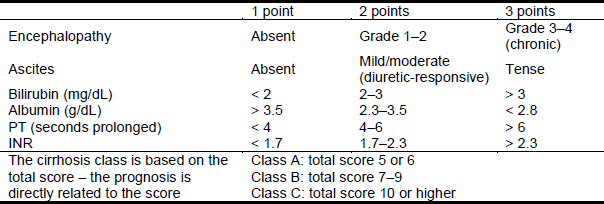
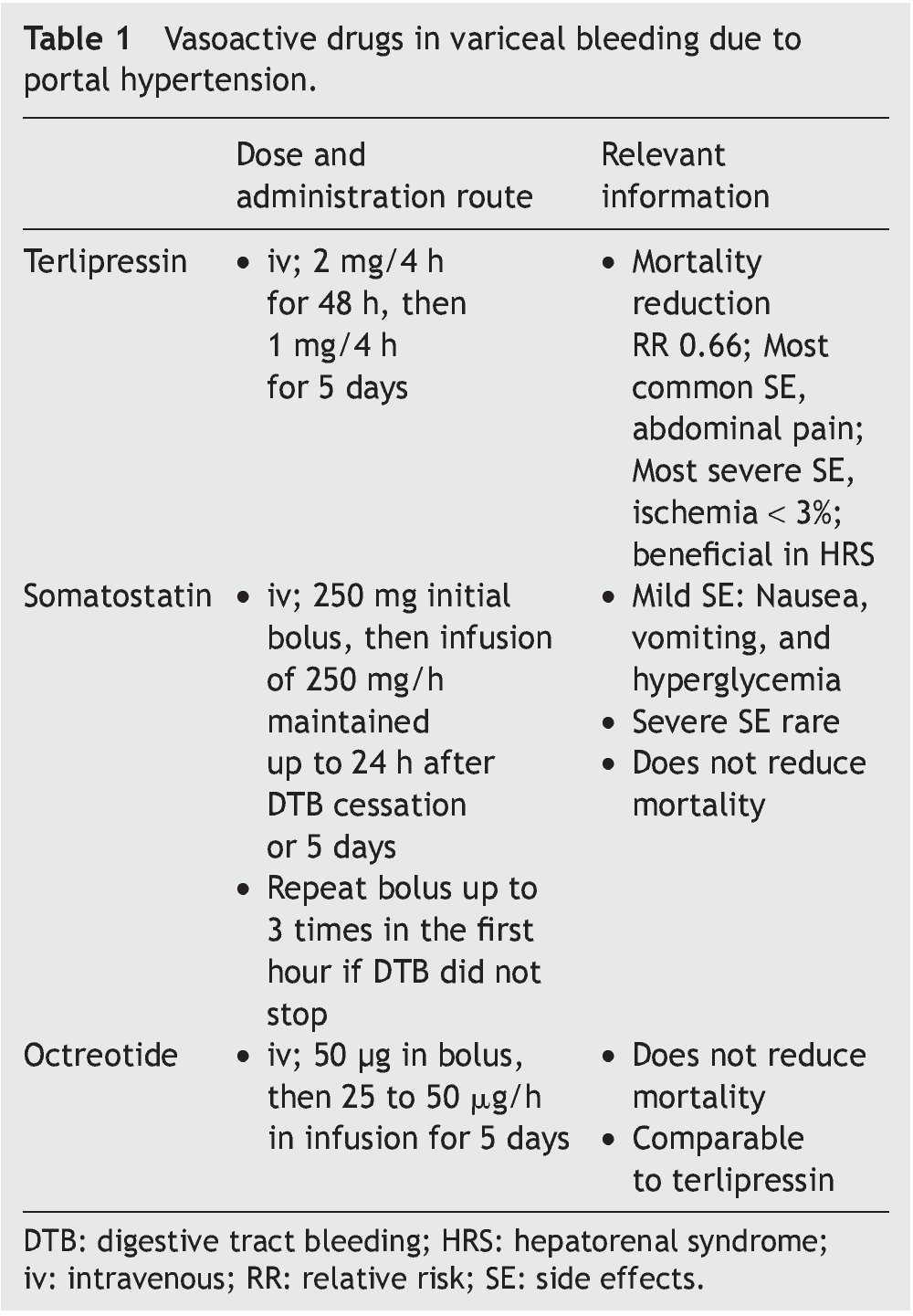
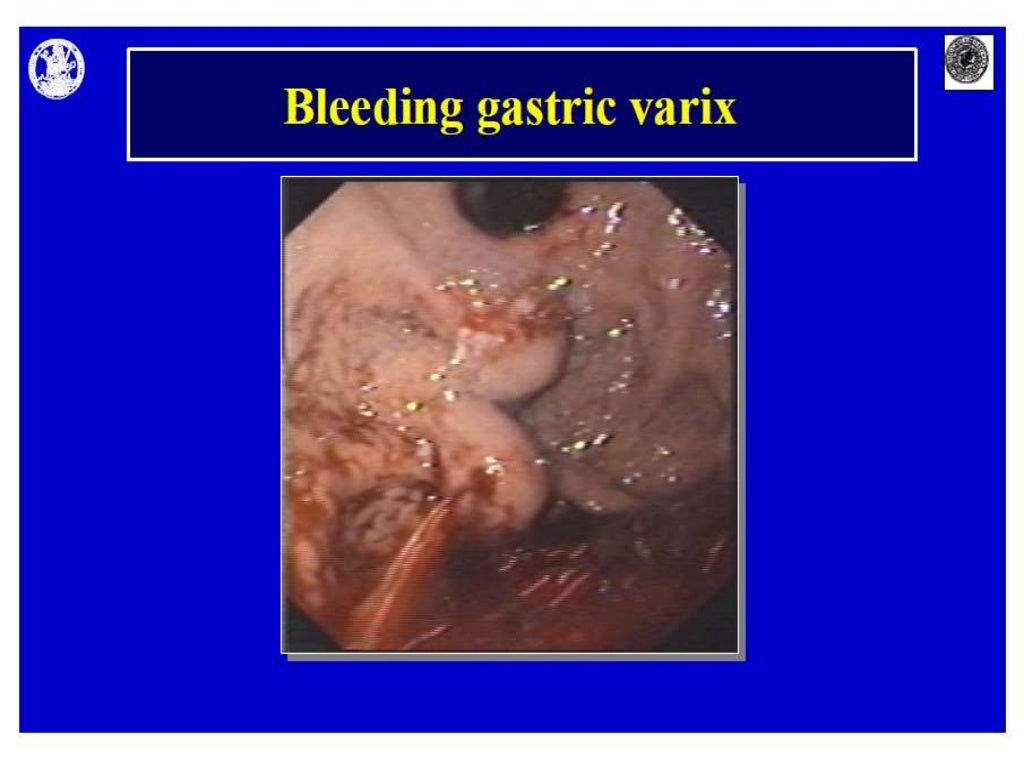
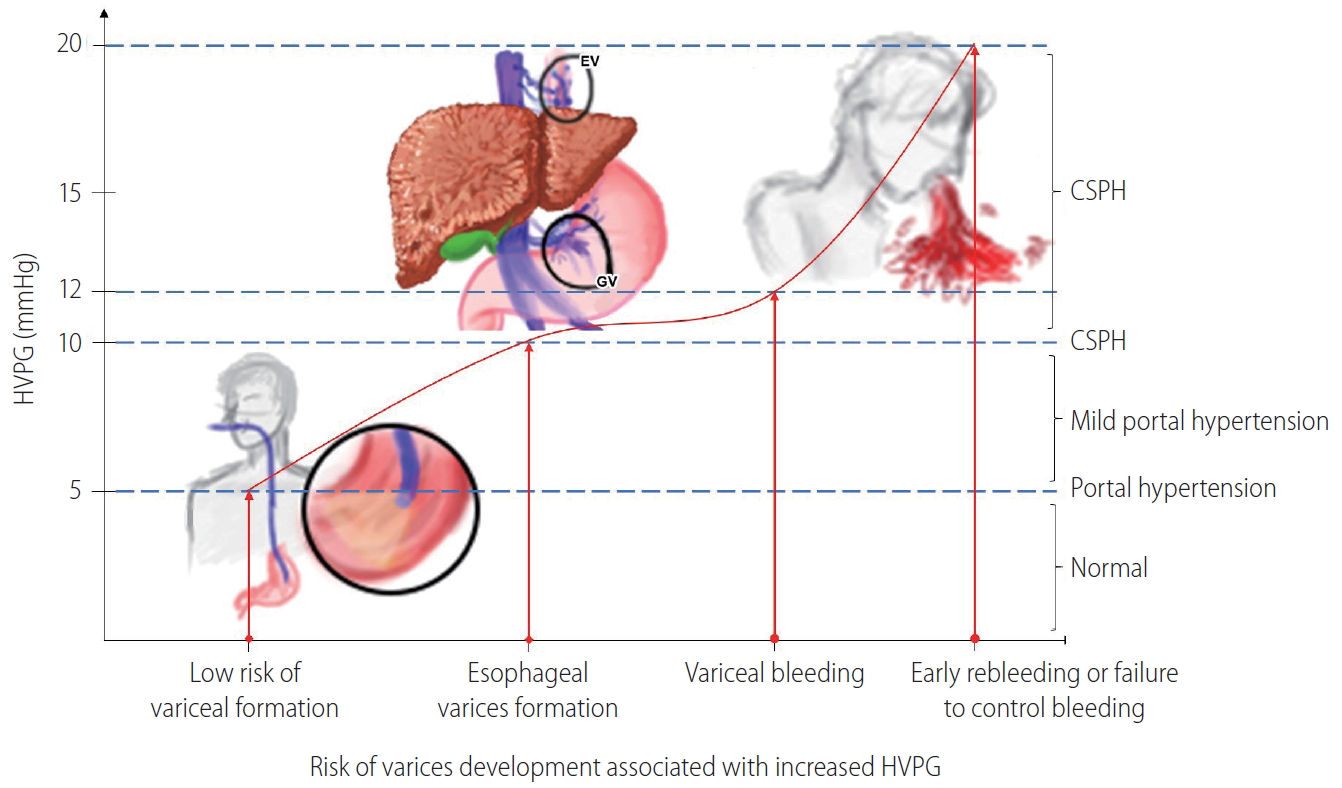
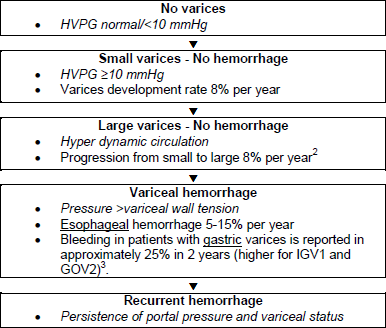
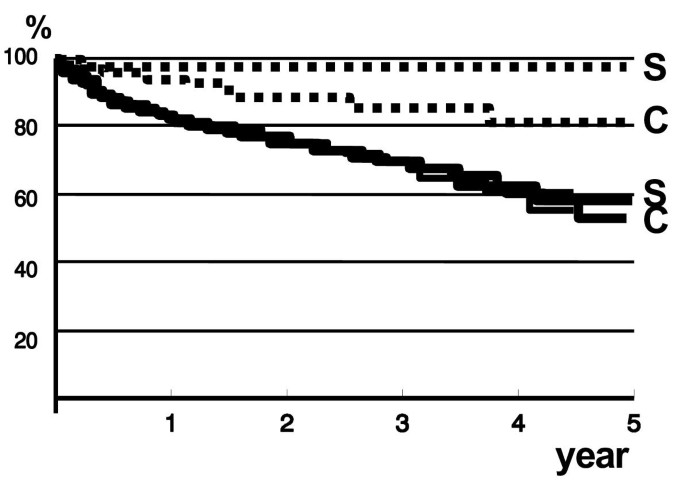
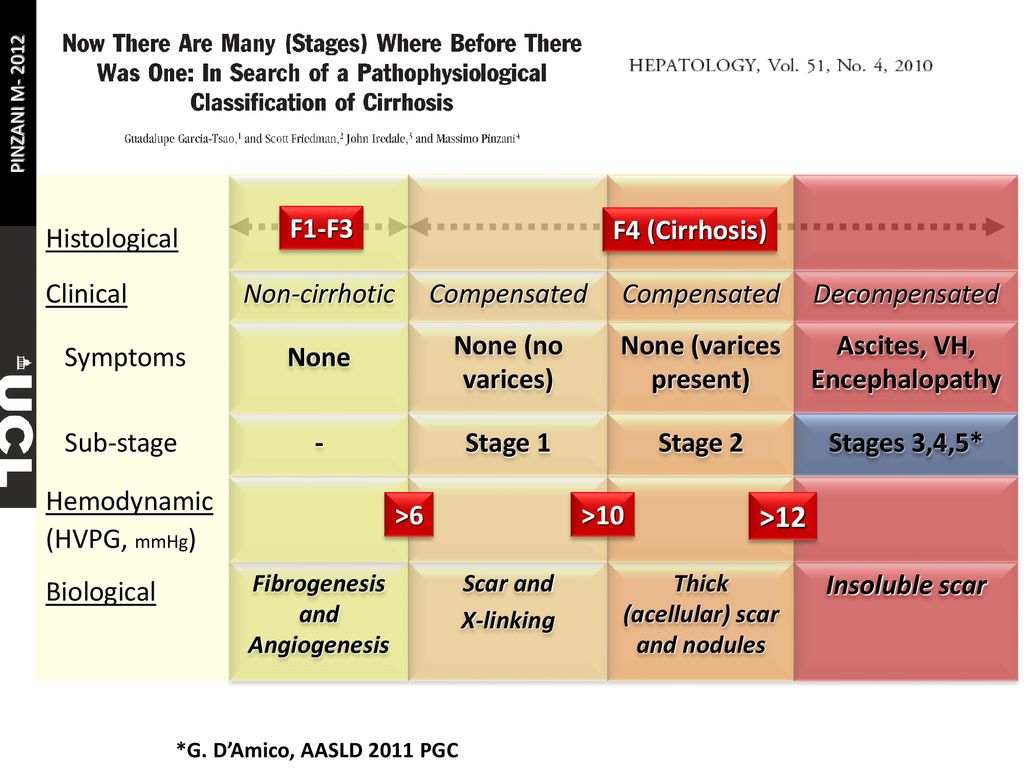
Synopsis of Inpatient Management for Esophageal Variceal Hemorrhage The authors suggest that all VH requires ICU admission with the goal of acute control of bleeding, prevention of early recurrence, and reduction in 6week mortality Imaging to rule out portal vein thrombosis and HCC should be considered HepaticVenous Pressure Gradient (HVPG) greater 1 Introduction Cirrhosis is often complicated by the development of portal hypertension Depending on the severity of liver disease as determined by the ChildTurcottePugh (CTP) classification, between 50% and 80% of patients with cirrhosis will ultimately develop esophageal or gastric varices Because of the significant morbidity and mortality associated with bleeding from varicesGastroesophageal varices (GEV) and variceal hemorrhage (VH) are clinical milestones in the natural history of cirrhosis, as they are closely related to the severity of portal hypertension and define specific stages in disease progression Variceal hemorrhage is a lifethreatening complication of ci
Gastric varices occur in about 5%33% patients with portal hypertension (less prevalent than esophagealIn 1 year if decompensated No betablocker prophylaxis Small varices (From Wikipedia, the free encyclopedia Esophageal varices are extremely dilated submucosal veins in the lower third of the esophagus They are most often a consequence of portal hypertension, commonly due to cirrhosis People with esophageal varices have a strong tendency to develop severe bleeding which left untreated can be fatal
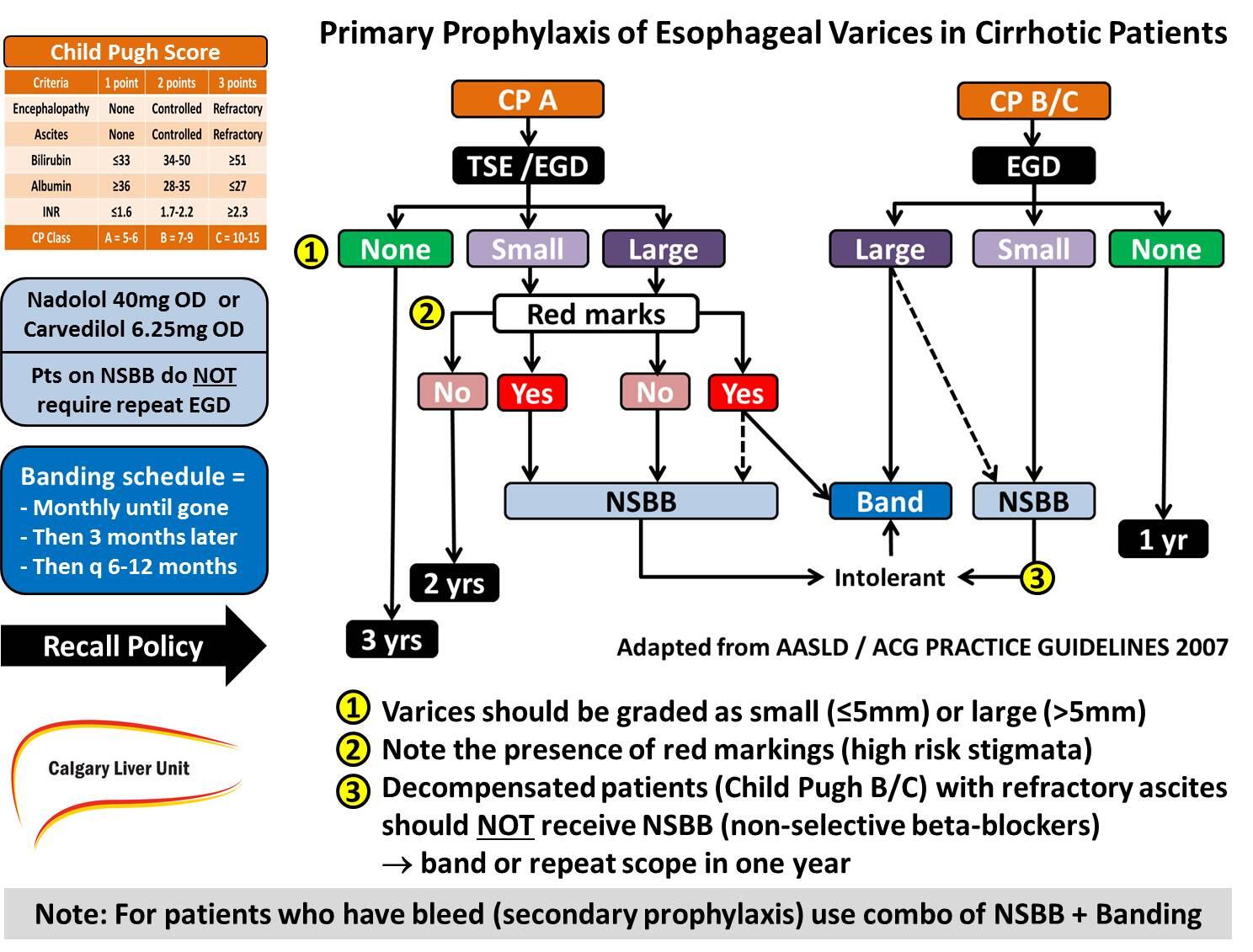
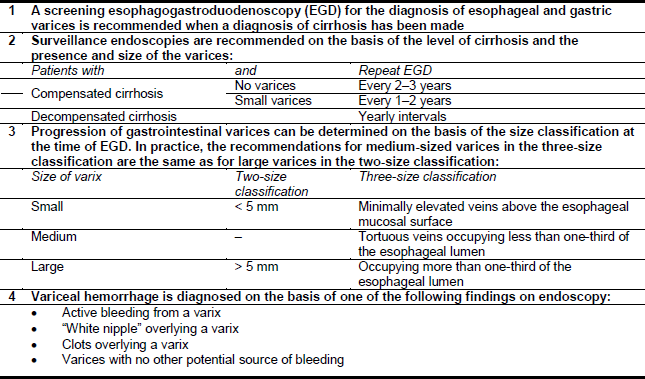
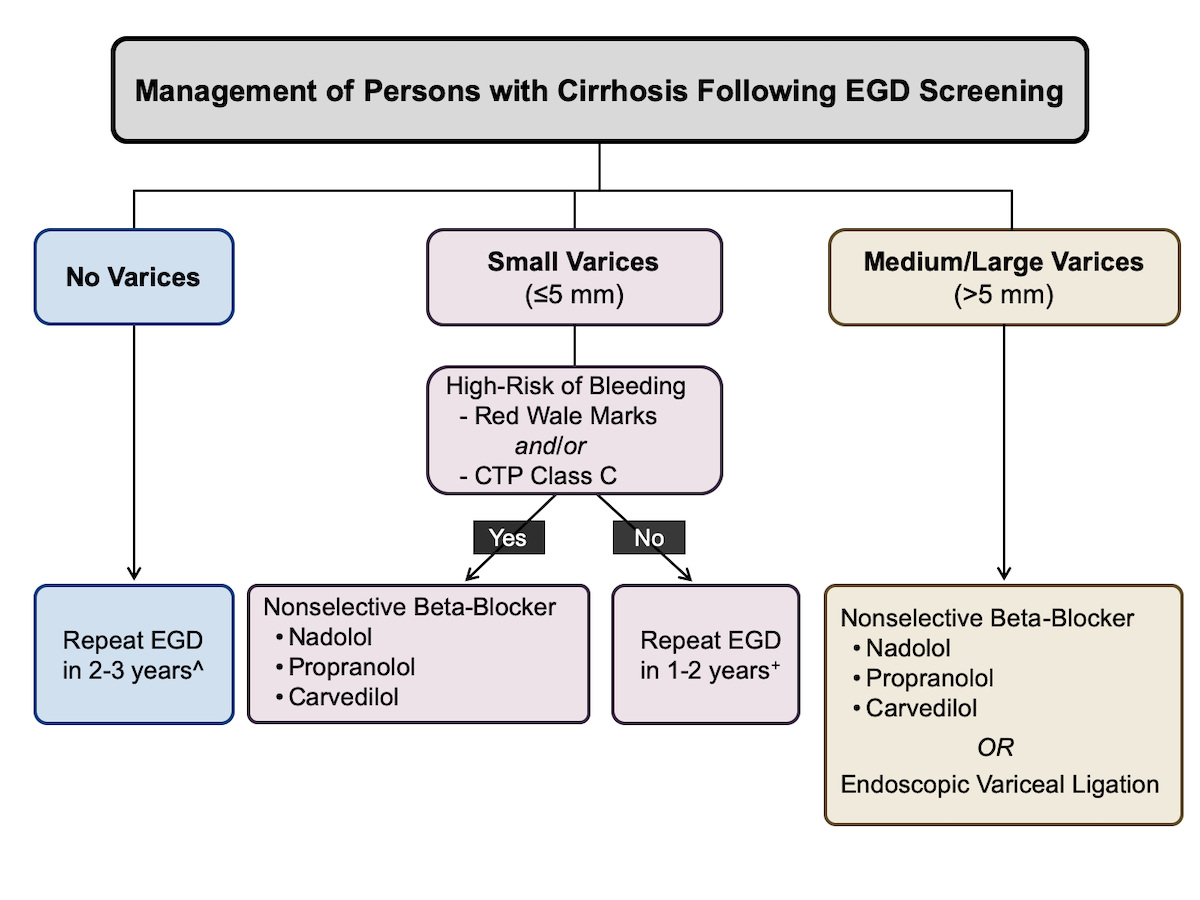
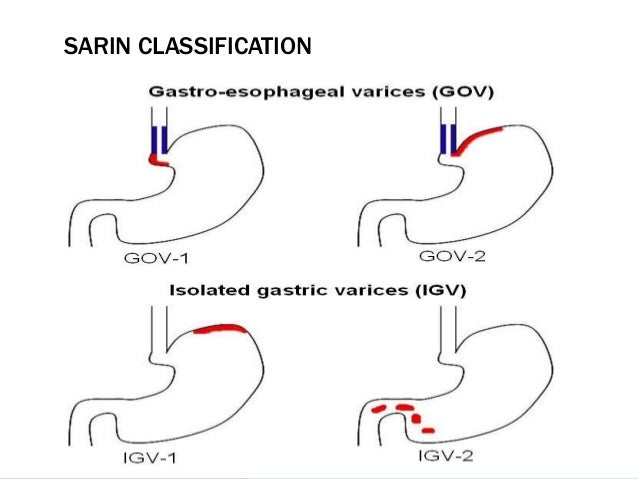
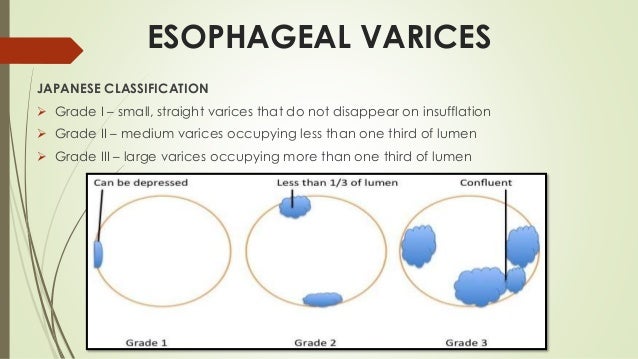
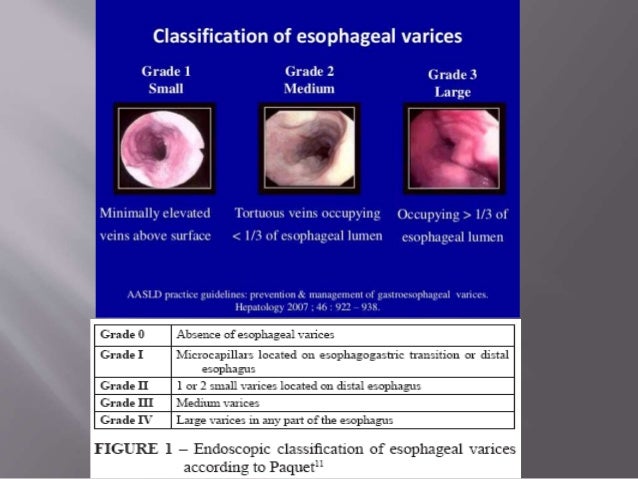
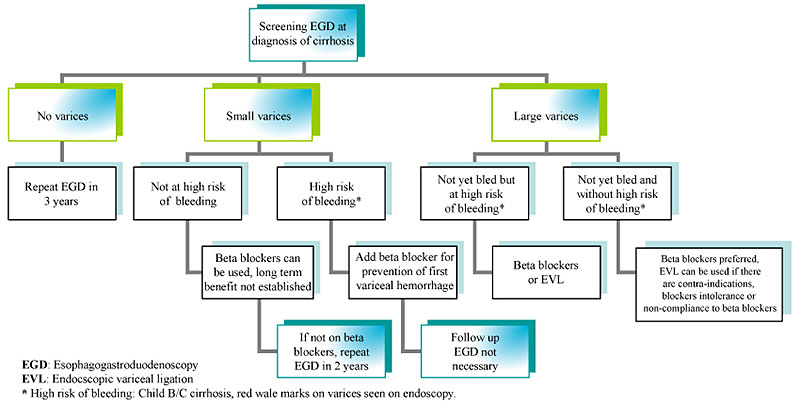
A screening esophagogastroduodenoscopy (EGD) for the diagnosis of esophageal and gastric varices is recommended when a diagnosis of cirrhosis has been made 2 Surveillance endoscopies are recommended on the basis of the level of cirrhosis and the presence and size of the varices Patients with and Repeat EGDOn EGD, esophageal varices should be graded as small or large (>5 mm) with the latter classification encompassing mediumsized varices when 3 grades are used (small, medium, large) The presence or absence of red signs (red wale marks or red spots) on varices should be noted (Class IIa, Level C)Most commonly used classification is Sarin's classification of GV SARIN'S CLASSIFICATION Gastric varices are categorized into four types based on the relationship with esophageal varices, as well as by their location in the stomach Figure 17 a Gastroesophageal varix (GOV) type 1 Extension of esophageal varices along lesser b




Mortality Risk Factors And Disparities Associated With Esophageal Variceal Bleeding In Children S Hospitals In The Us The Journal Of Pediatrics




Practice Guidelines sld
PURPOSE To prospectively evaluate the accuracy of esophagography with barium in diagnosis of esophageal varices (EV) in patients with compensated cirrhosis, with endoscopic gastroduodenoscopy as the reference standard MATERIALS AND METHODS In this study, which was approved by the local Helsinki Committee and in which all patients consented to participate,Varices are categorized based on their appearance and size Per AASLD guidelines, varices should be classified into one of two categories small or large Small varices are those that are 5mm in diameter Some institutions utilize a three category classification basedMeasures to prevent recurrent variceal bleeding such as eradicating esophageal varices and improving liver function are important for reducing the risk of mortality This topic will discuss the prevention of recurrent bleeding from esophageal varices in patients with cirrhosis Management of other complications of cirrhosis and portal



View Of Non Invasive Screening For Esophageal Varices In Patients With Liver Cirrhosis Annals Of Gastroenterology



Screening For Varices And Prevention Of Bleeding Core Concepts
The most commonly used and perhaps the easiest for endoscopists is the American Association for Study of Liver Disease (AASLD) two‐grade classification system with a cutoff of 5 mm that divides them into small or large 2 There is also a third‐grade system that uses a score of small, medium and large, but in reality, medium and large are managed the same way, thus theACG & AASLD Joint Clinical Guideline Prevention and Management of Gastroesophageal Varices and Variceal Hemorrhage in Cirrhosis Guadalupe GarciaTsao, MD,1 Arun J Sanyal, MD,2 Norman D Grace, MD, FACG,3 William D Carey, MD, MACG,4 the Practice Guidelines Committee of the American Association for the Study of Liver Diseases and the Practice ParametersThe issue for measuring the varix size F1 smallcaliber varices, not disappear with insufflation F2 Moderately enlarged, beady varices, less than 1/3 of the esophageal lumen F3 Markedly enlarged, nodular or tumorshaped varices, more than 1/3 of the esophageal lumen World J Surg 1995; On EGD, esophageal varices should be graded as small




Practice Guidelines sld




Schematic Showing The Recommendations From Major International Download Scientific Diagram
Medium and Large Esophageal Varices The 16 AASLD practice guidance on Portal Hypertensive Bleeding in Cirrhosis classifies medium and large varices in the same category for variceal bleeding prophylaxis recommendationsCC, varices develop at a rate of 7%8% per year,(10) and progression from small to large varices occurs at a rate of 10%12% per year, with decompensated cirrhosis being an independent predictor of progression() VH occurs at a rate of around 10%15% per year and depends on the severity of liver disease, size of varices,Screening for esophageal and gastric varices, prevention of variceal bleeding, and the management of patients with variceal hemorrhage7 ESOPHAGEAL VARICES Screening for esophageal varices Effective prophylactic treatments exist for patients with esophageal varices to prevent variceal bleeding8 There are



Http Www Kasl Org Pdf 14 Liverweek Day1 B 3 Clinical hepatology update 2 1 Ea B9 80 Ec 81 Ea A0 Pdf



Www sld Org Sites Default Files 19 10 sld Asge Endoscopycourse Sessioniii Pdf
AASLD Practice Guideline 07 Management Cirrhosis Screening and surveillance No varices Repeat endoscopy in 3 years (well compensated);The AASLD 1998 recommends endoscopic screening in patients with Child B and Child C liver classification Esophageal varices was assessed in accordance with the OMED classification as follows12 degree esophageal varices was found in 10 subjects (278%), 2nd degree in 23 subjects (639%), and 3rd degree in 3Esophageal varices bleed is the cause of death in one third of these patients Re bleeding occurs in about 25 percent to 30 percent due to esophageal varices in a span of 2 to 3 years4 Cirrhotic patients have 5% incidence of esophageal varices / year5 AASLD recommends that upper GI endoscopy should be done in these patients for evaluation of




Oesophageal And Gastric Varices Classifications Pdf Document



Kelly Warren Burak Calgary Liver Unit Approach To The Prophylaxis Of Esophageal Varices In Cirrhotics Based On sld Acg Guidelines Http T Co 2ilw4ycwkd
Prevalence, classification and natural history of gastric varices a longterm followup study in 568 portal hypertension patients Hepatology 1992 Dec 16(6) MedlineThe 5 functional esophageal disorders Take Quiz Does mild hypertriglyceridemia increase pancreatitis risk?Gastric varices are less prevalent, occurring in 5% to 33% of these patients Variceal hemorrhage occurs at a yearly rate of 5% to 15% The most important predictor of hemorrhage is the size of varices;



Www Cghjournal Org Article S1542 3565 19 X Pdf




Endoscopic Management Of Oesophageal And Gastric Varices Intechopen
Gastric Varices Gastric varices are less prevalent than esophageal varices and are present in 5%33% of patients with portal hypertension with a reported incidence of bleeding of about 25% in 2 years, with a higher bleeding incidence for fundal varices38 Risk factors for gastric variceal hemorrhage include the size of fundal varicesBackground & Aims The American Association for the Study of Liver Diseases recommends the use of a 2grade classification system (small and large) todescribe thesize of oesophageal varices (OV) Data on observer agreement (OA) on this system are currently lacking We aimed to evaluate this classification and compare it to the widely used 3grade classification (grade 1The larges varices are at highest risk of bleeding Other predictors of hemorrhage are decompensated cirrhosis (Child B/C) and the endoscopic




Endoscopic Management Of Oesophageal And Gastric Varices Intechopen




Role Of Eus Evaluation After Endoscopic Eradication Of Esophageal Varices With Band Ligation Gastrointestinal Endoscopy
Background & Aims The American Association for the Study of Liver Diseases recommends the use of a 2‐grade classification system (small and large) to describe the size of oesophageal varices (OV) Data on observer agreement (OA) on this system are currently lackingPreprimary prophylaxis of varices Primary prophylaxis of varices Patient with cirrhosis and small esophageal varices In highrisk small esophageal varices, NonSelective βBlocker (NSBB) should be used In lowrisk small esophageal varices, NSBB may be used if desired by the treating physician Nitrates alone or in combinationNew varices develop in about 5%15% patients per year, enlarge by about 4%10% per year 2;




Primary Prophylaxis Of Esophageal Variceal Bleeding Simonetto 12 Clinical Liver Disease Wiley Online Library



Esophageal Varices Primary Prophylaxis And Prevention And Management Of Rebleeding Springerlink
AASLD practice guidances are developed by a panel of experts on a topic, and guidance statements are put forward to help clinicians understand and implement the most recent evidence Recently AASLD has published guidances on aspects of a topic that lacked sufficient data to perform systematic reviews Many guidelines published before 14 are Gastric varices are dilated submucosal collateral veins that develop in the setting of portal hypertension due to any etiology with or without cirrhosis1 Compared to esophageal varices, gastric varices are less common occurring in approximately % of cirrhotic patients However, gastric varices have a higher propensity to bleed severely and are often associatedEsophageal varices are Portosystemic collaterals — ie, vascular channels that link the portal venous and the systemic venous circulation They form as a consequence of portal hypertension (a progressive complication of cirrhosis), preferentially in the sub mucosa of the lower esophagus



Www Idsociety Org Globalassets Idsa Topics Of Interest Emerging Clinical Issues sldguidelinehccupdate10 1 Pdf




Endoscopic Management Of Oesophageal And Gastric Varices Intechopen
For individuals who have recovered from an episode of acute esophageal VH, the AASLD for bleeding oesophageal varices Br J to ChildTurcottePugh classification in predicting outcome AASLD GUIDELINES FOR GE Varices Recommendations for Diagnosis 1 Screening EGD for the diagnosis of esophageal and gastric varices is recommended when the diagnosis of cirrhosis is made (Class IIa, Level C) 2 On EGD, esophageal varices should be graded as small or large (>5 mm) with the latter classification INTRODUCTION Upper gastrointestinal (GI) variceal bleeding is associated with significant mortality in cirrhosis The prevalence of variceal bleed is known to occur in %50% of patients with cirrhosis, with rebleeding as a significant cause of death1,2For the past 30 years, the mortality has improved markedly from intensive use of endoscopic therapies, vasoactive



Esophageal Varices Primary Prophylaxis And Prevention And Management Of Rebleeding Springerlink



3
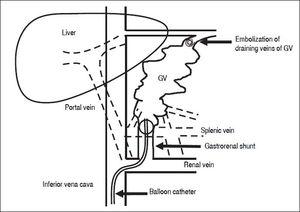
The endoscopic treatment of choice for esophageal variceal bleeding is band ligation of varices Bleeding from gastric varices is treated by injection with cyanoacrylate Treatment with vasoactive drugs as well as antibiotic treatment is started before or at the same time as endoscopy Bleeding from portal hypertensive gastropathy is lessAASLD Transplant Hepatology Board Review Course bleeding esophageal varices Use parenteral nutrition when energy needs cannot be maintained by oral/enteral methods oConsider parenteral nutrition with unprotected airways and HE when cough and swallow reflexes are compromised (EASL)




Easl Clinical Practice Guidelines For The Management Of Patients With Decompensated Cirrhosis Journal Of Hepatology




Practice Guidelines sld



Spleen Stiffness Probability Index Sspi A Simple And Accurate Method To Detect Esophageal Varices In Patients With Compensated Liver Cirrhosis Annals Of Hepatology




Evaluation And Management Of Esophageal And Gastric Varices In Patients With Cirrhosis Clinics In Liver Disease




Algorithm For Screening For Esophageal Varices And Primary Prophylaxis Download Scientific Diagram




Prospective Randomized Trial Endoscopic Follow Up 3 Vs 6months After Esophageal Variceal Eradication By Band Ligation In Cirrhosis European Journal Of Internal Medicine



English World Gastroenterology Organisation




Practice Guidelines sld




Ectopic Varices Sarin 12 Clinical Liver Disease Wiley Online Library



Portal Hypertensive Bleeding Abdominal Key




Oesophageal And Gastric Varices Historical Aspects Classification And Grading Everything In One Place Abstract Europe Pmc



Management Of Gastroesophageal Varices In Cirrhotic Patients Current Status And Future Directions Annals Of Hepatology




Ct Esophagography Non Invasive Screening And Grading Of Esophageal Varices In Cirrhosis Topic Of Research Paper In Clinical Medicine Download Scholarly Article Pdf And Read For Free On Cyberleninka Open Science



Oesophageal And Gastric Varices Classifications



Variceal Hemorrhage Cleveland Clinic



Developments And Controversies In The Management Of Oesophageal And Gastric Varices Gut




Improved Survival In Patients Receiving Medical Therapy As Compared With Banding Ligation For The Prevention Of Esophageal Variceal Rebleeding Lo 08 Hepatology Wiley Online Library



Http 49 231 15 21 Deptweb Cdownload Php Dl Id 409 Dl Name Surgf Pdf




Sarin Classification Of Gastric Varices Adapted From Sarin Et Al 69 Download Scientific Diagram



Esophageal Varices World Gastroenterology Organisation




The Baveno Vi Criteria For Predicting Esophageal Varices Validation In Real Life Practice



Screening For Varices And Prevention Of Bleeding Core Concepts




Clinical And Molecular Hepatology




Ct Esophagography Non Invasive Screening And Grading Of Esophageal Varices In Cirrhosis Sciencedirect




Esophageal Varices Grade វ ជ ជ អ ហ មស ភ រម យ Facebook



1




New Frontiers In Liver Resection For Hepatocellular Carcinoma Jhep Reports



Esophageal Varices Primary Prophylaxis And Prevention And Management Of Rebleeding Springerlink




Screening For Varices And Prevention Of Bleeding Core Concepts




A Commonsense Approach To Esophageal Varices Clinics In Liver Disease



Www sld Org Sites Default Files 19 10 sld Asge Endoscopycourse Sessioniii Pdf



1




Randomized Controlled Trial Of Scleroligation Versus Band Ligation Alone For Eradication Of Gastroesophageal Varices Gastrointestinal Endoscopy



English World Gastroenterology Organisation



Is Endoscopic Therapy The Best Choice For Primary Prevention Of Variceal Hemorrhage In Patients With Liver Cirrhosis



1
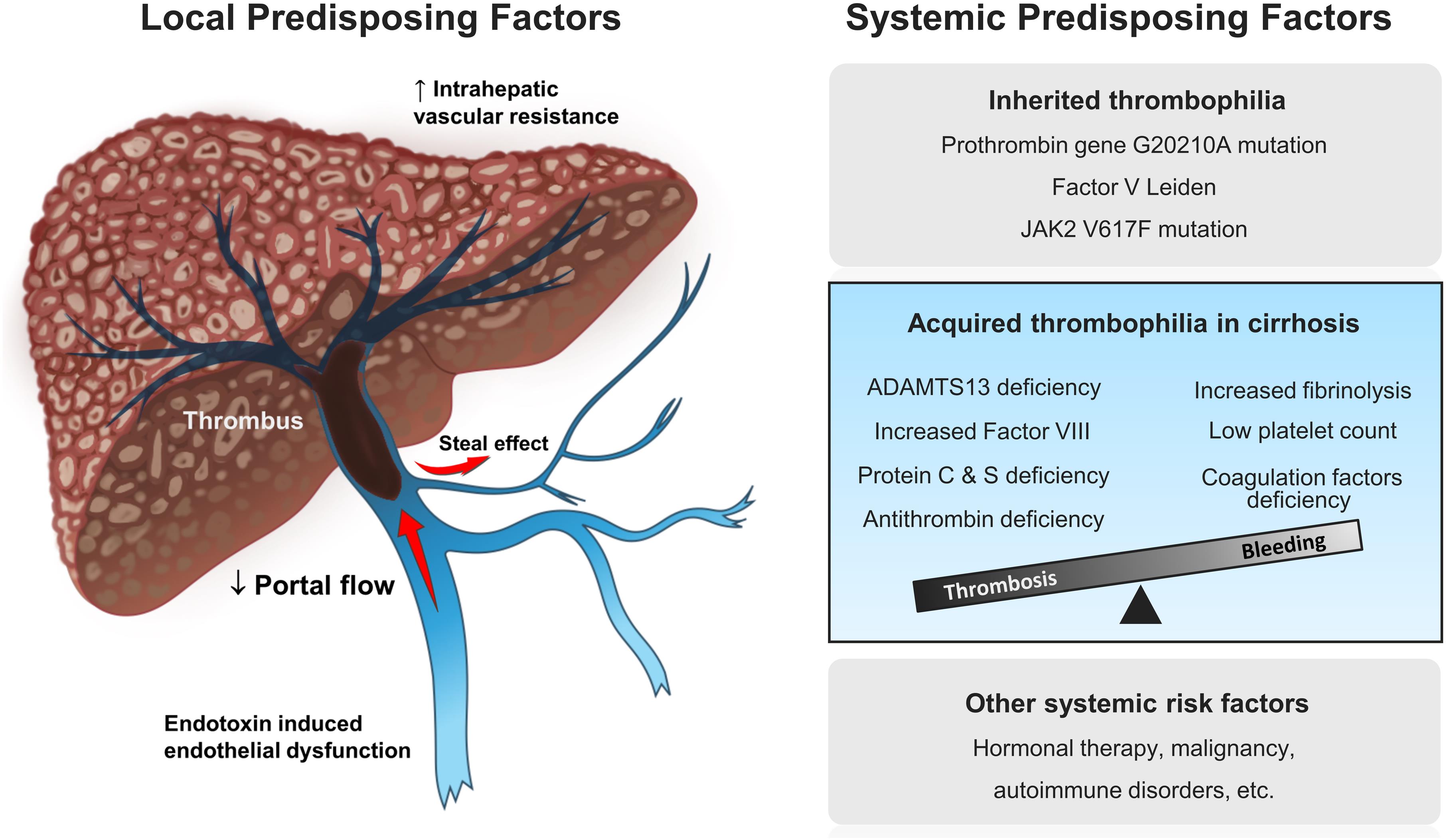



Nontumoral Portal Vein Thrombosis A Challenging Consequence Of Liver Cirrhosis




Portal Hypertensive Bleeding In Cirrhosis Risk Stratification Diagnosis And Management 16 Practice Guidance By The American Association For The Study Of Liver Diseases Garcia Tsao 17 Hepatology Wiley Online Library



Www sld Org Sites Default Files 19 10 sld Asge Endoscopycourse Sessioniii Pdf



Screening For Varices And Prevention Of Bleeding Core Concepts



Louisville Edu Medicine Departments Medicine Divisions Gimedicine Physician Resources Lectures Other Disorders Of The Small And Large Intestine Variceal Bleed Pdf



English World Gastroenterology Organisation




Endoscopic Treatment Of Gastric Varices Clinics In Liver Disease



Oesophageal And Gastric Varices Classifications



Institutional Experience With Cyanoacrylate Treatment Of Gastric Varices




Endoscopic Treatment Of Acute Gastric Variceal Bleeding In Patients With Cirrhosis Using Isoamyl 2 Cyanoacrylate Fouad Ta E Shabaan E J Med Sci Res




Algorithm For Screening For Esophageal Varices And Primary Prophylaxis Download Scientific Diagram



Upper Gi Bleeding




Xuxwbwrjrjv7m




Adherence To sld Guidelines For The Treatment Of Hepatocellular Carcinoma In Clinical Practice Experience Of The Bologna Liver Oncology Group Digestive And Liver Disease




Validation Of The sld Recommendations For Classification Of Oesophageal Varices In Clinical Practice Fateen Liver International Wiley Online Library



Mexican Consensus On Portal Hypertension Revista De Gastroenterologia De Mexico




34 Portal Hypertension Varices Gastropathy And Gastric Antral Vascular Ectasia Abdominal Key



Esophageal Varix Disease Malacards Research Articles Drugs Genes Clinical Trials



Http Www Reevax Com Embolization04 Pdf



Oesophageal And Gastric Varices Classifications



Www sld Org Sites Default Files 19 10 sld Asge Endoscopycourse Sessioniii Pdf




Therapeutic Gastrointestinal Endoscopy Semantic Scholar



Www sld Org Sites Default Files 19 06 Garcia Tsao Et Al 17 Hepatology Pdf




Figure 8 From Portal Hypertension Pre Primary And Primary Prophylaxis Of Variceal Bleeding Semantic Scholar



Cmh Clinical And Molecular Hepatology Clin Mol Hepatol 2287 2728 2287 285x The Korean Association For The Study Of The Liver 10 3350 Cmh 0022 Cmh 0022 Review Managing Liver Cirrhotic Complications Overview Of Esophageal And Gastric




Declining Hospitalization Rate Of Esophageal Variceal Bleeding In The United States Clinical Gastroenterology And Hepatology




Easl Clinical Practice Guidelines For The Management Of Patients With Decompensated Cirrhosis Journal Of Hepatology




Pdf Correlation Of Thrombocytopenia With Grading Of Esophageal Varices In Chronic Liver Disease Patients Amanullah Abbasi Academia Edu




Practice Guidelines sld



Gi Bleeding Presentation



Variceal Hemorrhage Cleveland Clinic



Www Hepatitisc Uw Edu Pdf Management Cirrhosis Related Complications Varices Screening Prevention Bleeding Core Concept All




Uk Guidelines On The Management Of Variceal Haemorrhage In Cirrhotic Patients Gut



Managing Liver Cirrhotic Complications Overview Of Esophageal And Gastric Varices



English World Gastroenterology Organisation



Oesophageal And Gastric Varices Classifications



Medicina Free Full Text Current Approaches To The Treatment Of Gastric Varices Glue Coil Application Tips And Brto Html



How To Manage Gastric And Ectopic Varices Springerlink



Endoscopic Sclerotherapy Compared With No Specific Treatment For The Primary Prevention Of Bleeding From Esophageal Varices A Randomized Controlled Multicentre Trial Isrctn Bmc Gastroenterology Full Text




Esophageal Varices Wikipedia



The Need Of A New Pathophysiological Classification Of Cirrhosis Ppt Download




Clinical And Molecular Hepatology




Oesophageal And Gastric Varices Classifications



Www Cghjournal Org Article S1542 3565 19 X Pdf



Mexican Consensus On Portal Hypertension Revista De Gastroenterologia De Mexico




A Pathophysiologic Gastroenterologic And Radiologic Approach To The Management Of Gastric Varices Gastroenterology



Www sld Org Sites Default Files 19 06 Garcia Tsao Et Al 17 Hepatology Pdf




Gastroesophageal Varices Cancer Therapy Advisor



0 件のコメント:
コメントを投稿